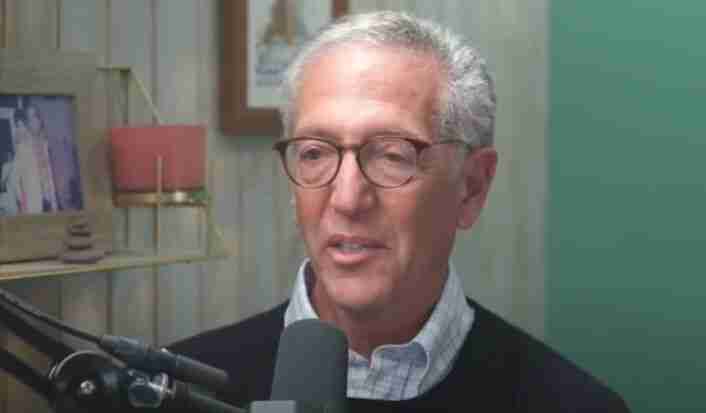
Read the full transcript of Dr. Rangan Chatterjee interviewing Dr. Howard Schubiner on “The Best Ways To Heal Chronic Pain & Trauma Without Medication”, Nov 9, 2022.
TRANSCRIPT:
Understanding Chronic Pain
DR. RANGAN CHATTERJEE: The research you have done around chronic pain I think is game-changing. I think it’s helping so many practitioners, it’s helping so many patients all over the world find healing where previously there was stress and heartache. So right at the top, what is chronic pain? What do those two words mean? And how common is it?
DR. HOWARD SCHUBINER: Yeah, well, everyone’s experienced pain and we need pain. Pain is a protector. Pain is something that it turns out our brain creates and generates.
So what I say to all of my patients, pain is a discomfortable experience basically, but it’s also an emotion. And so when you get down to it, we kind of think is every time someone has pain that there must be something wrong with their body. And it turns out, as we’ll discuss, the vast majority of people who have chronic pain actually don’t have a structural problem in their body.
Most people with acute pain probably do because if you break an ankle or something. And if you break an ankle, you want pain because it tells you, it’s a message that your brain is giving you to stop, don’t walk on a broken ankle. But it turns out if you have a broken heart, you might get chest pain, but it might be due to your brain giving you the message that there’s something amiss, there’s something wrong in your life.
And so what I say to all my patients is you can’t understand pain unless you understand how the brain works. So we start with that because it’s a much broader view of understanding pain that we can get into.
DR. RANGAN CHATTERJEE: Yeah, when you say acute pain versus chronic pain, what does that mean? And do you have some examples of common conditions or syndromes or diagnoses that fit under this chronic pain diagnosis?
Common Chronic Pain Conditions
DR. HOWARD SCHUBINER: Yeah, for sure. Take headaches. In the US, 25 million people suffer with chronic headaches.
And so if you have headaches, you think there must be something wrong. There is something wrong, you have pain. But it’s chronic.
It’s not like you hit your head and you have an injury to your forehead and it hurts and it’s going to go away in a couple of days or you have a tumor or an infection or a bleed. As physicians, we know there’s certain structural problems that cause headaches. But the vast majority, 95, 98% of people with chronic headaches don’t have a structural disorder.
They go to the doctor, they get their CAT scan or MRI, they get tested for their sinuses, their teeth, their ears, their mouth, etc. And there’s nothing wrong. So what’s the cause?
It’s chronic headache pain, what we call primary headache, right? So what’s the cause of that? Most doctors say, well, genetic or I don’t know or whatever.
And what we’re saying is we know exactly why people have chronic headaches because we can talk to them, we can listen to them, we can hear their story and we understand how the brain works and how the brain can create a cycle of pain due to neural circuits that get activated due to stress and emotions in life situations. And then it continues to get activated by this vicious cycle of pain leading to fear of pain which leads to more pain.
The Medical System’s Approach to Chronic Pain
DR. RANGAN CHATTERJEE: You know, I reflect back on my career to date and I remember early on as a primary care doctor some of the most frustrating cases were those patients who would come in with chronic pain, whether it be chronic migraines, headaches, bilateral arm pain, you know, whatever it might have been. Because as a medical doctor, certainly back then as a very junior medical doctor, I didn’t really feel I had the tools to help these people.
As I say that, Howard, I remember distinctly one afternoon I was in Timperley. I was in a practice in Timperley. I can remember this lady coming in, maybe 60, 62. You know, she would smoke 15 or 20 cigarettes a day. She was really struggling with life. She was on a whole host of painkillers. You know, I had all these letters from the pain clinic. You know, just increase the pregabalin by 25 milligrams.
I remember seeing her thinking, everything we’re doing, nothing’s working. And all I’ve got is a specialist letter telling me to increase the dose of a pain medication by 25 milligrams, even though nothing’s working anyway.
And I wish I could go back to that patient now knowing what I know through your research, through my own clinical experience. I wish I could go back and help that lady because I think she’s an example of, A, that patient is struggling and suffering, okay? But I also think doctors, I think they feel really powerless and frustrated with cases like that.
And I think what ends up happening in my experience is that the patient often feels that they haven’t been heard. This guy, this woman, whoever it be, this healthcare professional is not taking me seriously.
DR. HOWARD SCHUBINER: We are spending billions and trillions of dollars for Band-Aids. We’re talking about Band-Aid care, put something over it as opposed to look and find the underlying cause. And the pain that is experienced in chronic headache and migraine and irritable bowel syndrome and fibromyalgia and chronic pelvic pain, and we’ve done research and looking at the causes of these, and most people with neck and back pain, we’ll talk more about that in a minute.
The pain they experience is real. It’s not imaginary. It’s not in their head. But it is in their brain because of neural circuits in their brain when the doctors can’t find anything wrong, which is the case most of the time as you’ve experienced.
They can say, oh, have this surgery or do this to fix it. That’s not going to happen. But they can get better.
And that’s the work that we’ve been doing. And a lot of other people are doing as well. But it starts with understanding the person.
It’s listening to them and understanding them and getting to know them and understanding what’s going on in their life so they can see what are the things which led to this situation. And they can know that you’re not invalidating them. You’re not stigmatizing them.
You’re not blaming them. That the pain is real and that they can get better. What a hopeful message as opposed to the incurable message that are mainly given by so many doctors and groups that are working in that space.
How the Brain Creates Pain
DR. RANGAN CHATTERJEE: This idea that when we experience pain, most of the time there’s nothing actually structurally going on in our body. I think it’s quite profound for people because I think we grow up with the understanding that if we have pain, there’s a physical cause of that pain. And you mentioned earlier on that the brain creates this experience of pain.
You mentioned something that I think most people, many people have experienced when they have a broken heart. They can literally feel a pain in their hearts, right? But nothing physical has actually happened.
So, help us understand that. What’s going on? How does the brain generate this experience of pain? And why does it do it as well?
DR. HOWARD SCHUBINER: Yeah, yeah, it is amazing. The book that I recommend to people is How Emotions Matter by Lisa Baird, a neuroscientist in the States. And there’s some very famous British neuroscientists, Friston and Clark particularly, have written about this extensively.
Their work is a little harder to read. It’s very deep. But this is emerging neuroscience of how the brain works.
Well, how does the brain work? Our brain creates what we experience. How do we see? We don’t see with our eyes. We don’t. Light comes in our eyes. But the light impulses have to be transformed electrically through the visual cortex to create the images that we see. And so, our brain creates what we see. And part of it occurs in what we expect to see.
The other day, I was driving by my friend’s house. I hadn’t seen him in a while. He was on vacation. I drove by. He’s standing in his doorway. It’s like, oh, wow, he’s home. Awesome. I drive up to the drive, knock on the door. There’s no one home.
My brain created the image of him standing there, basically a hallucination. And police officers, this is controversial. My wife doesn’t like me to talk about it. But they go to the scenes of crazy stuff, especially in the States. And they have to say, do I see a gun or not? Well, sometimes they see a gun that’s not actually there or vice versa.
If I gave you prism glasses that turn the world upside down, you’d see everything upside down, but only for a few days. And then your brain would switch the images to be right side up again because our brain creates what we see. Our brain creates what we hear.
The other day, I was at a meeting. A young woman got up and said, good morning, America, which is like, that’s a weird thing to say. She actually said, good morning, I’m Erica. But I didn’t know her name. But my brain was just latching on to something and creating something.
And so when you break an ankle, it’s not your ankle causing pain. An ankle can’t cause pain. When you touch a hot stove, it’s not your finger. The impulses go to the brain, but the brain decides, and this is the craziest thing, but it’s true.
Neuroscientifically, the brain decides whether to actually turn on pain or not, whether to give you the experience of pain or not. How do we know that? Because a lot of people and a lot of people that experience themselves, you get an injury and you have no pain at all.
So the brain decides whether to turn on pain or not. And it’s there to protect you. It’s something that everyone needs. It’s like a smoke alarm. And the research shows, neuroscience research shows, that emotions and stress activate the exact same parts of the brain as does a physical injury. And we can talk about why our brain might do that.
We don’t know for sure. But whether God created us that way or we evolved that way, but that’s how our brain works. So the pain that occurs due to a fracture is exactly the same as the pain that occurs due to a stressful situation that occurs in our life. It’s real pain and it can be severe pain. And that’s what people say, how can the pain be so frigging severe and not be due to a structural injury? It’s amazing.
But it’s true, we see it every day.
Healing Chronic Pain Without Medication
DR. RANGAN CHATTERJEE: Yeah, and that’s, I think, the power of a lot of your work, a lot of your research, is helping to give scientific validity to something that many practitioners have experienced, many patients have experienced, that emotional pain, emotional injury can totally manifest as physical pain. I have found, like you, Howard, I think that many cases, arguably the majority of cases with chronic pain, can be healed. In my experience, at least, I’d love your view on that, without using any medication, if you take time to help the patient understand what’s going on, get to the root cause.
I mean, what would you say to that?
DR. HOWARD SCHUBINER: Exactly, it’s 100% true. And we have data now showing that. I can talk about that in a second.
But the most important thing is that it’s not all in your head. When a doctor says, or anybody says, it’s all in your head, it’s cruel. And it’s ignorant, because it implies that it’s their fault, that they want the pain somehow, that they’re crazy or mentally deficient, you know, or making it up. And none of that is true at all. And so that validation is so important.
The Invisibility of Emotional Pain
DR. RANGAN CHATTERJEE: I guess, you know, you can look at it this way, if someone had a physical injury, like we could see, let’s say their ankle, and it was red, it was hot, it was swollen, and they were hobbling for a few weeks and had to, I don’t know, take crutches to work with them. People would be sympathetic, they could see that, they could understand, yeah, oh, and you need some help, you know, I get it, you’re in pain, right? We have an understanding of that.
But a lot of emotional pain is hidden. We can’t see it. The people around you can’t see it. So therefore, one of them we have sympathy for, as a society, the other one, we kind of ignore.
DR. HOWARD SCHUBINER: Right, and we’re not really looking at the whole person. So if you take, for an example, it’s kind of a common story, right? You take a young woman, say, whose father was critical, yelling and screaming sometimes.
Maybe alcoholic, kind of that sort of thing. And she grows up with this sense that life isn’t safe, that people are unpredictable. People in my life are unpredictable around me and can yell or scream at me, or even worse.
And then she grows up, and then when she’s 15, she has a boyfriend, and then he betrays her, cheats on her, sends pictures of her around the school, or something like that, and then she gets migraine headaches. Do you have sympathy for her? Of course you do.
And then she’s in her 20s, and she marries a guy who happens to be kind of like her father, kind of maybe abusive, or maybe harsh with the children. And then she starts getting irritable bowel syndrome or pelvic pain. Do we have sympathy for her?
And then when she’s 35, she divorces the jerk, but still not paying child support or whatever. And then she gets in a small car accident, and then her neck starts to hurt, and it gets worse, and then her whole back starts to hurt. And then she starts to feel anxious or depressed, and then maybe she gets pain all over, and they say she’s got fibromyalgia.
And now at the end of this, she feels completely broken. And people maybe are looking at her like, you know, just get on with your life. What’s wrong with you?
Nothing. Do we have sympathy for that person? Are you kidding me?
Understanding Chronic Pain
DR. HOWARD SCHUBINER: Her whole life has been one which cries out for understanding and cries out for her to be heard, listened to, respected, cared for. And when you look at it that way, yeah, this pain is real. And all these pains are due to the stress that’s been caused in her life, none of which is her fault.
DR. RANGAN CHATTERJEE: When you use the term chronic pain, are you able to list some of those conditions that fall under that umbrella term? And I’ve got a reason for asking this, you mentioned headaches already, but if you could just sort of go down a common list, because I think this conversation and what we’re talking about is relevant to almost everyone, whether in their own lives or someone very close to them. And I wonder if you might just make it super, super clear for us who we’re referring to.
DR. HOWARD SCHUBINER: Well, chronic pain just means any pain that’s lasted for, you know, they say three months or six months as the definition. But the conditions that are commonly what I would call neural circuit-based pain, in other words, brain generated pain in the absence of structural problem are primary headaches, like tension and migraine headaches and other headache conditions like occipital neuralgia, trigeminal neuralgia. Most people with TMJ problems do not actually have problems on the x-ray, but when you talk to them and take their history and take time, TMJ pain, most of the time is neural circuit-based or mind-body type pain.
If you take people with costochondritis, chronic chest pain, again, in the absence of heart disease or lung disease, most people with, the vast majority of people with irritable bowel syndrome and what’s called non-ulcer dyspepsia. If you take people with chronic pelvic pain, they may be diagnosed as having pudendal neuralgia or pelvic floor dysfunction or vulvodynia, but all those things are just names. They’re just describing that you have chronic pain.
Fibromyalgia? Fibromyalgia, absolutely. We did a study of chronic neck and back pain, and we haven’t published it yet, but a colleague I have in the States examined 220 consecutive patients coming into his clinic with chronic neck and back pain.
He’s a physiatrist, physical medicine physician, and he determined that 88% of them had non-structural pain. This is shocking because if you go to a doctor with chronic neck or back pain or a chiropractor or a massage therapist or a physical therapist, they’re going to say, oh, well, you have degenerative disc disease. Look, it’s on the x-ray or the MRI.
You have got bulging discs, but everyone has those. And if you look closely at the data, we can share this data with you and your listeners. The vast majority of people have those things on x-ray, as I do in my neck, without pain at all.
And so we have to be very clear and very careful what we’re talking about. And everyone needs a very careful evaluation, but those are the main conditions. But the brain can produce anxiety and depression when we’re under stress, obviously.
The brain can produce fatigue that can be severe and overwhelming. And we see that all the time. The brain can produce eating disorders.
The brain can produce, well, we can talk about lung COVID as well, of course. So there’s just so much. The fact is, is that if you’re, the reason that my patients and your patients have these conditions is because they’re human.
They’re just human. They have a brain. They have a body.
They react to stress that occurs in life. And everybody has some of these. Everyone does.
I like to say when I started my internship, I was a young doctor. I got diarrhea for six months. Well, was that diarrhea real? Well, it’s real. You can see it. But it wasn’t because I had something wrong in my bowel. I was scared, being a young doctor and making mistakes and hurting people. And I was just being human.
The Medical System’s Failure with Chronic Pain
DR. RANGAN CHATTERJEE: You know, what’s interesting about all those conditions that you’ve just listed is that almost without fail, I would say those are the conditions that we manage in medicine pretty poorly. I don’t think that’s controversial to say. I think patients know it.
We as medical doctors know it. Those are the conditions where it’s often, as I’ve already mentioned, quite frustrating because actually the tools with which we’re trained, the tools that we learn at medical school just don’t work that well. And this is, I guess, one of my biggest realizations as a doctor throughout my career has been how important the mind is in our lives, our physical health, our vitality, how much a role it plays.
But we are literally taught zero about that medical school. Now that could all speak because research was limited at the time when I was at med school. But I don’t see much evidence of that changing at the moment.
You know, when I’ve spoken to a mutual friend of ours, Gabor Mate, in the past, we, and Gabor talks a lot about trauma and how still in many medical schools, the trauma word doesn’t even come up at all in the entirety of medical education. And now that we know how much early life trauma affects our risk of autoimmunities and all kinds of other conditions later on in life, it’s baffling as to why it’s taking this long for it to get into medical school training because doctors are getting frustrated, patients are feeling underserved. But that thing you just mentioned, Howard, about MRI scans, I think that’s a really great point to dive into.
I wonder if you could share some of those statistics.
DR. HOWARD SCHUBINER: If you take 30-year-olds, people in their 30s, and you do an MRI, these are people with no pain at all. 40% of them have degenerative disc disease. 30% have a bulging disc.
These are 30-year-olds. These are normal findings that occur with aging. So, what happens when you’re 50?
50-year-olds, 80% of people have degenerative disc disease with no pain. 60% have bulging discs with no pain. 30% have herniated discs with no pain.
DR. RANGAN CHATTERJEE: So, here’s the problem that I’ve seen as a medical professional, right? The patients there, they’ve either seen a specialist or got a scan. As the primary care doctor, you get the scan results and it will say, bulging disc at L4 or L5, right?
No nerve impingement or something. There’ll be some kind of report. And then you’ll say, or as a professional will often say, oh, the reason you have your pain is because of that disc problem on your scan.
And that’s a very dangerous thing to say to that patient, I think. What would you say to that?
The Danger of Misdiagnosis
DR. HOWARD SCHUBINER: Incredibly dangerous and maddening. Why maddening? Well, because it not only gives them the erroneous diagnosis, and also I want to talk to you more later about how we assess to make sure that we know that the bulging disc isn’t the cause of pain, but it’s giving them an erroneous diagnosis.
So, it’s making them think that there’s a problem that can’t be fixed or needs fixing with medication or injections or even surgery. And we see so much, maybe not quite as much here as in the States, but so many surgeries that are being done on people’s necks and backs for treating the MRI, not treating the patient. And there’s never been a randomized controlled trial showing that surgery for neck or back pain, axial pain is better than watching it or exercise or physical therapy or anything.
There’s no evidence that this is what we should be doing, but we’re spending billions of dollars. But it’s not that so much, it’s that it also makes people worse because what happens in the brain, we’ll talk more about this. What happens in the brain is that the more you’re fearful of it, every time, if you have back pain, the more fearful you are of it, it’s going to get worse over time because the neural circuits in the brain, you’re getting a positive feedback loop, whereas pain leading to fear, focus on it, worry about it, frustration with it, it actually makes it worse because that’s how those neural circuits work.
So it’s really not understanding the brain and not understanding the data, the scientific data we have about these MRIs because these abnormalities go up to 90% when you’re 60 and beyond, but these are people without any pain.
It’s like saying you’ve got wrinkles on your skin and that’s the cause of your headaches because you have wrinkles or that your hair is getting gray and that’s the cause of your migraines, that’s the kind of thing that we’re doing.
DR. RANGAN CHATTERJEE: And I think this is a key point how much for me, how we as healthcare professionals can unwittingly make the problem worse, because as you say, this can worsen things, this can create a fear. And it also, what we say as healthcare professionals, certainly as doctors, has real power. It can really positively or negatively influence what that patient believes, what they feel.
Like, let’s say they’re one of these many people who have abnormal MRI scans of their spine. They’ve got a bulging disc, let’s say. They probably had that for years, well before they actually had the pain.
Maybe that bulging disc has nothing to do with their pain at all. And then here’s the problem, the way I see it, is that if we say that to the patient, oh, yeah, oh, you know, we found the cause of your pain, that patient then goes out into the world with the belief, my spine, my disc is causing my pain. So everything they do after that is based on an erroneous belief system.
Whether they’re trying treatments or therapy or anything is all based on that truth. And that truth actually may not be true. Now, I wonder if I might share with you my own journey with, through and now beyond chronic pain.
Because I think perhaps if you hear that, you might be able to explain various bits along the way. Would that be okay?
DR. HOWARD SCHUBINER: Yeah, that would be great.
Dr. Chatterjee’s Personal Experience with Chronic Pain
DR. RANGAN CHATTERJEE: So I’m now in my early 40s.
DR. HOWARD SCHUBINER: Really? You look much younger.
DR. RANGAN CHATTERJEE: When I was in the final year of medical school, I was helping my flatmate at the time move into a new flat that we were all going to move into. And all afternoon, I was lifting heavy boxes out of a car. Probably with appalling lifting techniques.
I knew nothing about it at the time. I never had a problem with my back or anything. So I wasn’t thinking.
And at one point during the afternoon, I remember getting something out of the back. I had a sharp pain in my lower right back, dropped everything, and I just went onto the floor. That’s the first time, to my recollection now at least, that I experienced back pain.
Now, that led to maybe a 10-year history where the quality of my life was hugely affected. I started off against the doctor, the university doctor.
DR. HOWARD SCHUBINER: But what happened immediately? So you fell down, you had this acute pain, right?
And then did you get up and finish the work or did you have to stop for the day? And what happened in the next two or three days, if you recall?
DR. RANGAN CHATTERJEE: Honestly, I cannot remember with any degree of accuracy. I probably would have stopped. I may have sat down for a while.
I may have rested. Maybe I helped get the remainder of the boxes up. I don’t really know.
But all I remember now, at least, is that I went on a journey for several years where I would take painkillers. I would go and see a physio. You know, I remember I got referred to a physio.
I think I paid privately for loads of physio sessions, limited use. Again, I’m not here to have a go at physiotherapy. I’m just saying for me, I was doing some strengthening exercises.
DR. HOWARD SCHUBINER: But was the pain coming and going? Was it turning on? Was it turning off?
Was it there constantly?
DR. RANGAN CHATTERJEE: I don’t think it was there all the time. I think I would just have an awareness of it. If I sat down for too long, I think I’d feel it.
At some point in that journey, I think, I don’t know when that was, it was probably, I don’t know, something like 1999, 2000, something like that. I moved back to the northwest of England from Edinburgh in 2003 to help look after my dad. And I was having real problems.
Like I was a junior doctor at the time. I was really struggling sometimes with the long ward rounds and my back was really bothering me. I had to take time off.
And I think I once went to my GP and they referred me for an MRI scan. Or I actually think it was at the hospital I worked. I got an MRI scan there.
And this is the first time, and I give the spinal surgeon who had the consultation with me a huge amount of credit for this. This would have been back around 2003, 2004. There was a disc abnormality on my MRI scan and I would have been in my mid-20s, something like that.
And he said to me, yes, you have a disc abnormality, L4, L5, but you’ve got to understand that I could take 100 people off the street and your age, do an MRI scan on them, a lot of them would have the same scan issue and most of them would have no pain at all. So, to be fair to him, back then, he was basically saying this is a static scan. This simply cannot tell me if you have the pain.
Understanding Chronic Pain and Its Emotional Connections
DR. HOWARD SCHUBINER: Yeah. Well, first of all, the data of these MRIs being abnormal in people goes back to the 1980s. So, it’s not really all that new. We’ve been compiling over the years.
But the thing is, what happened at that initial moment? You might have twisted your back. You might have had a back injury due to lifting improperly or whatever. Or your brain might have said, you know, it’s been a long day, Rangan. You’ve been working really hard. Maybe this guy’s not really appreciative. Maybe he’s got too many boxes. Maybe they’re too heavy. You know, there’s a certain amount of stress going on and your brain might have said, time out, you know, you’ve got to stop doing this.
And your brain can’t talk to you. It doesn’t speak English. It can only speak in some kind of message. So, it might have sent a pain. So, in either case, the point is, you had pain in your lower back at that moment. And then you did the appropriate thing. You rested. And then you didn’t stress out about it too much. And you didn’t use your body too much. Then you gradually started to get back into action. And if it was an injury, it had healed.
Because all injuries heal. And so, if it was an injury, it healed. And then you would be fine. Unless the neural circuit for that pain continued. And what causes a neural circuit for pain to become chronic or to continue? It’s that memory of it. It’s the fear of it.
Next time you go to lift something, there’s a little subconscious reaction going on in your brain there. Uh-oh, be careful. Don’t lift. You might get pain again. And then that actually can cause that neural circuit to turn on pain. And then it can enlarge, not just to lifting, but to other stressful situations, like being on rounds for a long time, standing up for a long time, sitting for a long time. These can all become conditioned responses.
And so, the chance that, you know, you didn’t, you may have a little muscle pull or something minor like that, but that healed. Yeah. And then what happened is the pain became chronic because those neural circuits got activated and then reinforced over time.
DR. RANGAN CHATTERJEE: It’s so interesting looking back at that now with fresh eyes, with someone like you sitting in front of me. Because bit by bit, it became chronic and it would affect how I felt about myself. I would become fearful. Oh, I can’t lift. I know I can’t help anyone move. I can’t lift the sofa.
And then again, the narrative, you know, you’re six foot seven, you’re really tall. Of course, you’re going to have back pain. But I actually, there was a deep part within me how he thought, that’s just nonsense, right? I do not have to be committed to a life of backache. In my mid-twenties, because I’m, you know, mega tall, I just refused to accept. I thought there’s something going on here. I’m going to find the way to heal this. I’m not accepting that.
And I won’t get into the whole story necessarily, but there’s two particular things I wanted to share with you. One is that on this journey, I, like many people, spend a lot of money on different therapies because like, this is just, I can’t play squash anymore. I can’t sit for long periods of time. I can’t drive for more than an hour. Like all this kind of stuff was real. And for me, it was like, oh, it’s because you’re tall. You look at your posture. You look at all these things.
And again, I’m not saying they have no value ever, but I found this guy. It was a ski video actually, this chap called Gary Ward, who I’ve written about. He’s an incredible, incredible guy in terms of biomechanics. And I went to see him. I went to study with him. And he was basically saying to me that my right foot at the time was flat. And he said, Rangan, I didn’t feel your, and this is not exactly what he said word for word, but essentially that your right foot is stuck in pronation. It’s not, you know, I think we can help that right foot get better.
He gave me some five minute exercise to get my right foot going. And literally instantaneously, I felt relief in my lower back. And that continued for years. So I could get back to squash. I could get back to long drives. I’d still have tightness. It would still come back from various times, but that made a huge difference. So I thought I got my quality of life back. But even though it was significantly better, it was still there. It would still come on at times of stress, I would notice.
DR. HOWARD SCHUBINER: So now you’re getting to the heart of it.
The Emotional Connection to Physical Pain
DR. RANGAN CHATTERJEE: Now I’m getting to the heart of it because when I got the deep realization, so just a quick overview. When I was in second or third year at medical school, my dad became seriously ill with lupus. His kidneys failed. He was 15 years on kidney dialysis. That’s why I moved back in 2003 to the Northwest. That’s why I live where I live today because I was helping my mom and my brother look after dad for many years.
Now at my dad’s funeral in 2013. So the context again, my back had been good for a few years. Like I’d been back to doing stuff, playing squash, back to the stuff I wanted to do in my life. But I’d still feel it. I mean, this moment, my dad was cremated and I can still remember wearing my suits at the end of the service. I remember my dad’s coffin I could see it being bought out and it went into the, I don’t know the official term, like the oven.
I saw the door open. I saw the orange, the heat. And I am not kidding you, right? I can almost feel it now as I say it to you. As my dad’s coffin went into the oven, I could feel my back ease off. And I was like, I know that just happened. I wasn’t thinking about it. It wasn’t as like I was planning for this to happen. And I thought about that and I thought, oh my God, this is the weight of looking after my father.
I honestly felt as I analysed it afterwards, oh wow, in that moment where you knew that dad was literally going to be gone. But because his body’s about to be burned, there is no more dad. On some deep level, it was like, I knew I no longer need to care and take on that weight.
DR. HOWARD SCHUBINER: Well, you had fulfilled your obligation. You came here to do what you needed to do. And it was a great gift to your father and your family. And it was a great gift to you as a son. And it was a beautiful thing. But it was a hard thing. And you did it for many years. And when at that moment you realise I’ve fulfilled my obligation, I’ve done it. And you can relax to that degree. And that’s what happened in your back.
Emotions matter. Emotions are real. We are psychological human beings. And the connections between emotions and our physical body are very real. These are neural circuits that get ingrained, get built in, get activated, get turned on and off. And I just think it’s a beautiful process to understand because when we can understand that, we can understand ourselves and the people we love and care about. And as doctors, we can understand our patients.
And people can understand that the symptoms they’re getting in their bodies sometimes are really just a message. They’re a message from our brain telling us something, but we have to interpret it. And oftentimes, and this is really hard for some people to hear, but oftentimes they’re a blessing in disguise. They’re pointing us towards something that we need to do or we need to take care of.
If you’re in a situation in your life which is difficult and overwhelming, you need to change your job or change a spouse or change your relationship or set some boundaries or do something in your life, you may be having headaches or stomach pain or chest pain or back pain. And you have no idea why, but if you look deeply and you are open to understanding these simple concepts, you can see it and it’s very real.
DR. RANGAN CHATTERJEE: You’re touching on a concept that often comes up on this show. And I say this with compassion, with, I hope, a great deal of sensitivity. But many people have shared with me when the mics are running, if they have got through to the other side of something, they’ll say, my disease was the best thing that happened to me. My cancer was my greatest teacher.
And again, these are people who have got through to the other side. So I understand if you’ve had cancer and you’ve had real problems with it and or someone’s had a friend or a family member who’s died from cancer. I understand that I’m not trying to in any way invalidate that. But what you’re really speaking to for me is this idea that our pain, our chronic pain is a signal. And if we can get to the root cause of what that signal is, the learnings we’re going to get from that will not only help our pain, but it will help every other aspect of our life as well.
Pain as a Signal, Not the Problem
DR. HOWARD SCHUBINER: The pain is not the problem. It’s the solution. What a weird thing to say. It’s the solution that our brain has come up with to alert us to a problem. It’s a signal. It’s a message. And it’s a protector. It’s a guide.
Your brain is saying like, look, I’m worried about you. There’s all this stuff going on. I’m worried about you. There’s something wrong. There’s something amiss. And here’s a signal for you to stop. Stop doing what you’re doing. Stop and think. Stop and evaluate. Whatever the message is.
And oftentimes, I remember there was a woman, I was on a video call with a bunch of people. A young woman was having neck pain. And it had started when she was in her university days. And I just asked her to close her eyes and put her hand over her heart and think about that person who was her, you know, eight or 10 years ago, whatever it was. And think about what that person, what she needed, what she was going through, what was happening in her life at the time that the neck pain started.
And she just started to cry, you know, because she felt compassion for herself. A lot of people have trouble with that, right? She felt compassion for herself at that age and what she was going through and how much pressure she was putting on herself and how hard she was working and other things that were going on in her life. And all of a sudden, it made sense to her why she got the neck pain at that time. And what happened as she started to cry, as she had her hand over her heart, as she was turning those tears into compassion for herself, neck pain disappeared. Just like that. It’s amazing.
DR. RANGAN CHATTERJEE: You mentioned that it’s important to properly evaluate a patient who’s suffering with chronic pain because of course there might be a structural component that is amenable to some sort of treatment.
DR. HOWARD SCHUBINER: Yes, of course.
DR. RANGAN CHATTERJEE: And, you know, related to that, you mentioned the brain is what creates the pain. Do we need to sort of outline what happens, right? What happens when we touch a hot stove? Is it worth us kind of unpicking that to help people understand that?
How Pain Works in the Brain
DR. HOWARD SCHUBINER: Yeah, for sure. The signals that go to the brain go up through the peripheral nervous system, through the spinal cord, into the brain, into several centers of the brain. And the different centers of the brain have different functions. Somatosensory centers and emotional centers and thought centers and memory centers. All those things are activated when you get these kinds of nerve signals coming up to the brain.
And there’s an immediate, and this is all subconscious. You’re not thinking like, oh, I hit myself. Oh, should I get pain or not? You can’t think that. It’s not a conscious process. It’s all happening on a subconscious level. And so most of the time when you have an injury, the brain will immediately turn on that pain as a signal. Just stop. Stop doing what you’re doing. Get help. Swear. You know, do whatever you have to do to take care of yourself. So that’s what happens in an acute injury.
But sometimes those signals are overridden. In an acute injury, the brain may not activate pain because there’s something else going on. You know, I like to say, if you’re running across the field and you break an ankle, you’re likely to get pain. If you’re running across the field and break an ankle, but you’re being chased by a lion, you probably wouldn’t get pain in that situation. So there’s a decision mode that’s going on in the brain that can override that.
The point is, is that injuries that occur, that cause pain, which is almost all the time, those injuries heal because our body always heals. But what happens is, is that sometimes the danger signal of what’s going on in people’s lives is also activated through memory, through prior injuries, through stress that’s going on in our life, that can activate this danger signal to make the pain continue, even though the injury heals.
So we see this all the time. That’s why I was asking you, like, what happened in the aftermath of, you know, hurting your back initially? Did the pain go away for a while and then it started coming back? Well, if the pain went away for a while and started coming back, chances are the injury healed. This makes sense.
Understanding Neural Circuits and Pain
DR. HOWARD SCHUBINER: But the neural circuits had been learned by the brain and then had gotten activated. So the brain learns, has this pathway that sometimes becomes a default pathway of neural circuits that keeps turning on pain every time you wake up in the morning or every time you bend over as a conditioned response. And so then those neural circuits become activated sometimes all the time or coming and going or in whatever pattern occurs.
But those neural circuits are real and they’re causing real pain, but it’s not because of the injury. So that’s the critical thing that we and physicians and PTs and everyone need to understand – to look carefully, to really listen to people about what happened with the injury, what happened with the healing and what is the history of the pain. Because if the pain is turning on and off structurally, if you break your arm, the pain doesn’t turn on and off.
DR. RANGAN CHATTERJEE: Yeah.
DR. HOWARD SCHUBINER: If you go away on vacation, it goes away and you come back to work, it comes back again. That’s a neural circuit problem. If the pain is triggered by stress, if the pain is triggered by the wind or cold or the weather, you know, there’s all these signs and clues that we have as physicians and other professionals to listen to people intently and make sure that we’ve ruled out a structural problem.
I’m a physician, we’re both physicians. You know, we know that the last thing we want to do is miss a tumor, miss an infection, miss an inflammatory condition, miss something. We desperately want to avoid doing that.
Context Matters in Pain Perception
DR. RANGAN CHATTERJEE: Yeah, as you say that, I think about Irritable Bowel Syndrome. IBS, super, super common. And for years, it was that diagnosis of exclusion.
Oh, well, you’ve got these problems, these stomach cramps, this constipation, this diarrhea, you know, bloating, whatever it might be. But your scans are all fine. The bloods are all fine.
Oh, you must have Irritable Bowel Syndrome. But there’s something inherently wrong with that sort of phraseology, because we’re not giving weight to the fact that, look, you’ve got really bad symptoms that are affecting the quality of your life. And from a physical standpoint, okay, we’ve ruled out the serious stuff.
Okay, that’s great news. But now we need to start digging into the emotional stuff. What’s been going on in your life?
Like we miss out that part. So the initial part happens, oh, there’s nothing seriously wrong with you. But actually, that’s very condescending, because actually, what do you mean?
You know, for many patients, what do you mean there’s something physically wrong with me? I can’t go to work. I have to open my bowels 20 times a day.
It’s awkward for me at work. It’s socially embarrassing. But the doctors are saying, there’s nothing wrong with you.
Do you know what I mean? So I think this is such a big point. You said about if you’re running across a field, and you hurt your ankle, whether your brain decides to give you a pain signal is going to depend on the context.
But I think that’s really powerful. Like if the context is a lion is chasing you, your brain, which is always trying to predict the future based on the past, is going to be like, hey, we have no time for pain. I need you to keep running now.
Whereas if you can stop, it might go, hey, listen, you know, let’s give him pain so that he stops. Like, is that an oversimplification?
DR. HOWARD SCHUBINER: No, no, that’s…
DR. RANGAN CHATTERJEE: Is that what happens?
DR. HOWARD SCHUBINER: That’s exactly what happens.
DR. RANGAN CHATTERJEE: Compare that to endurance running, right? Or endurance events. Because I think many people may be familiar with this experience of, I don’t know, people always say like David Goggins, this former, I think, US Navy SEAL in America, who’s known for doing all kinds of ultra endurance events.
I think he has said something to the effect of when you think you can’t go on, you’re not even 40% of the way there. In terms of you’ve got so much capacity left that you don’t even know. Now, I don’t know if that’s based on science or just his viewpoints, but I think that kind of fits in here.
The Power of Self-Talk
DR. HOWARD SCHUBINER: Yeah, Tim Noakes is an exercise physiologist from South Africa. And he’s written about this and he calls it the governor. Yeah, there’s a governor and it’s like up there.
And at some point you’re hitting the wall. At some point you’re saying, oh, I can’t go on, I can’t go on. But it’s a feeling.
It’s a protection. Again, the brain is protecting you. It’s saying like, hey, why are you doing that?
You know, it’s way too much. You know, you can’t handle it. Everyone talks to themselves.
All great athletes talk to themselves, but everyone talks to themselves. If you think you’re not talking to yourself, you’re the one who’s crazy because we’re always giving ourselves messages. And if we’re saying to ourselves, oh, my back is always going to be bad, that’s a message that’s making the brain make it worse and worse over time.
If you’re saying to yourself, I can’t handle this marathon or I can’t handle this 5K or whatever, that message is going to affect how you feel and how tired you are and how much you can run. Literally, we’ll do that because the brain has power over our muscles and over our sensations and over our feelings. That’s just how the brain and the body work.
And so if we can really understand and great athletes understand it, they know say, oh yeah, I know, I know. I’m really tired. That’s okay.
I can handle this. And then they keep going.
Personal Experience with Back Pain
DR. RANGAN CHATTERJEE: It’s just so fascinating to me. Another thing just came up there, Howard, from literally a few weeks ago. So I consider myself for many years now to not have a back problem.
I will lift beds, sofas. I’m not limited in anything I do anymore because of my back. It was a long journey.
I’ve shared with you some of the things of that journey, therapy, IFS, which we may talk about and other things, this kind of holistic approach to my own healing has massively helped, I’m sure. Listeners of the show will know that I’ve spoken about my mum several times. Mum’s quite elderly now.
She’s very immobile. She needs a lot of care. And sometimes she’ll slip off the bed or have a fall.
And maybe the carer or often it’s me or my brother will go around and try and help mum and get her back on to the bed or get onto her chair. Now, what’s really interesting is even though my back has been healed for years, usually before I’d lift mum up, I would be thinking, oh man, I hope this doesn’t strain my back. Oh man, I’ve got something important this weekend.
I hope I don’t pull my back. You know, there’s this kind of almost self-fulfilling narrative before I do it. And invariably, the next day, I’d feel a bit of tightness and then it would go.
And sometimes it would last a few days and I’d be thinking, oh man, it’s because I lifted mum. Which kind of makes sense based upon the narratives that we pick up. But a few weeks ago, this is exactly what happened.
I was in my kitchen. I got a call from my brother. It was about 5 p.m. And he says, hey mate, are you around? Like mum slips off the bed. I need some help. I said, is mum okay? Is this an emergency? He goes, mum’s okay, but we need to get her up. It’s a few deep breaths.
And I thought, hey, Ronja, go around. Don’t show any stress. Be totally calm. This is not a bad thing. I’m lucky that I live nearby. I can go and help my elderly mother now. Like I reframed the narrative in my head. This is my self-talk. So I went in.
I said, hey mum, how are you doing? Oh, you’re sitting there on the side of your bed. You slipped off. And she had a little smile. She had a little giggle. Like in the past, I’ve gone around feeling quite anxious and quite stressed.
So I intentionally went in. And then I thought, before I lifted mum, I just said, hey, I’m a strong human. Honestly, this is what I said. I’m a strong, wild, resilient human. Lifting my mum is no problem. And I went in with a big smile on my face, got mum up, got her back into bed.
Again, this isn’t N equals one, Howard, right? I’m aware of that. But I’m sharing this because it really speaks to your experience. This was just a few weeks ago. I consider myself to no longer have back issues. But again, there’s a memory.
Oh, if I do this in an awkward position, it’s going to cause backache. But when I went in with complete stress-free, smiling on my face, telling myself I can handle this no problem, I felt nothing. So I think that speaks to what you just said.
Pain Reprocessing Therapy
DR. HOWARD SCHUBINER: So you just described what we would call pain reprocessing therapy. So when we treat people, if I can back up just a second.
DR. RANGAN CHATTERJEE: Please do.
DR. HOWARD SCHUBINER: When we evaluate people, we’re listening to their story. We’re validating them. We’re understanding them.
We’re looking at what symptoms they have and making sure there’s not a structural problem. And we’re listening to the symptoms they have and making sure that it is a neural circuit problem by the fact that it’ll turn on, that’ll turn off, it’ll shift, it’ll move, it’ll be triggered by innocuous things, it’ll be inconsistent. A whole variety of criteria that we use and that we’re using that back pain study that I described earlier.
And then we’ll look for any emotional stuff that might be going on or has gone on in their life that may have contributed to it. So we do all that. And then we decide, oh, this is a neural circuit problem.
This is amenable to reversing by two types of solutions. And the one solution that we’re calling pain reprocessing therapy and the other type of solution that we’re calling emotional awareness and expression therapy. So the first one dealing with the neural circuits in the brain directly and the second one dealing with emotions.
And in our Boulder back pain study, we evaluated, well, they were randomized controlled trial. There were 45 people randomized to our arm of the study. Of the 45, I evaluated all of them. Of the 45, 43 had nothing wrong with their back. Structurally. Structurally, nothing wrong.
They had MRIs were abnormal, of course. But based on all the history, as I described, this was a neural circuit problem. 43 out of the 45. The other two, I’m not 100% sure about, again, being cautious. And so I could, and these people had an average duration of back pain of 10 years.
DR. RANGAN CHATTERJEE: Wow.
DR. HOWARD SCHUBINER: Now, of those people, 44 were treated. Of those people, 33 were pain-free in one month. So 75% of the people we treated were pain-free after 10 years of back pain in one month, simply using what we’re calling pain reprocessing therapy.
And you just described it to a T.
DR. RANGAN CHATTERJEE: Really?
DR. HOWARD SCHUBINER: Because what is pain reprocessing therapy? It’s changing the narrative. It’s thinking about yourself differently. It’s thinking about the back differently.
It’s understanding why it’s there. And it’s understanding that it is a neural circuit. It’s having hope that it’s reversible because it is.
And then it’s, as you go to lift or bend or move, you’re telling yourself, I’m okay. I’m safe. I’m not in danger.
And you’re smiling. I mean, you did it. And when you smile and when you give your brain reassurances, you’re turning off that danger alarm mechanism that is the actual cause of the pain.
And so for these folks, we didn’t go into emotional issues. We didn’t go into their past. We didn’t deal with their emotions at all.
We just changed the narrative. Changed the narrative. And how powerful that was to have 75% of people pain-free in one month.
I mean, that’s amazing. There’s never been a study with chronic back pain or any chronic pain that’s shown that kind of result.
DR. RANGAN CHATTERJEE: Yeah, that’s incredible. 75% better after a 10-year history in 30 days.
DR. HOWARD SCHUBINER: Yeah.
DR. RANGAN CHATTERJEE: It’s incredible. And I hope that that gives people listening and watching to this hope that actually no matter how long you’ve been suffering, there may well be something you’ve not tried yet that could help. Now, again, do you face much skepticism from people about this?
You know, what’s the pushback? Where does that pushback come from? I know this is real because I…
DR. HOWARD SCHUBINER: It’s massive.
DR. RANGAN CHATTERJEE: Yeah, because I’ve also… Again, I did that. I didn’t know it was pain reprocessing therapy.
I didn’t know I was doing that on myself. I was just based on everything I’ve learned, everything I’ve seen with patients. It’s like, you don’t need to have the same experience.
You can change your experience of the same events. But yeah, where does the pushback come from?
DR. HOWARD SCHUBINER: Well, you did that because you felt that you could.
DR. RANGAN CHATTERJEE: Yeah.
DR. HOWARD SCHUBINER: You were saying, I don’t have a back problem. That’s step one. And then it’s talking to yourself with this positive. I mean, it sounds silly to talk to yourself, you know, give yourself affirmations.
How stupid is that? But those have been shown in FMRI studies of the brain to change the brain. Our brain is neuroplastic. And when you’re giving yourself these positive messages, and then you start, we use a graded exposure technique where you start to maybe move a little or even imagine yourself moving with joy. Imagine yourself moving with a smile. Imagine yourself moving with these messages of safety.
And we do this right in the office. And I’ve got videos of folks in my office where they’re having pain with bending over. And then I have them imagine bending over. And then it hurts and say, oh, you’re imagining bending over and it hurts. Your brain is afraid of you bending over. Oh yeah, that’s what’s happening.
Healing Chronic Pain Through Mind-Body Connection
DR. HOWARD SCHUBINER: And now tell yourself you’re safe and you’re not in danger and smile and bend over five degrees and then 10 degrees. And pretty soon they’re bending over because those neural circuits are changeable because it’s not a structural problem. It’s amazing that we see this happening on a oftentimes really quick basis, not always, but oftentimes.
DR. RANGAN CHATTERJEE: You know, it’s interesting that as you were describing that, the name Eliud Kipchoge came to mind for you. Are you familiar with Eliud Kipchoge? He’s a Kenyan marathon runner.
From what we know, he’s the fastest marathon runner of all time and with help from his sponsors and a lot of pacers, he actually broke two hours for running a marathon maybe a year ago, something like that. But why that came to mind, even though I don’t think Eliud talks about pain, describes pain. In fact, I’d love your comments on this.
When he’s running, because I was watching that sub two-hour marathon race with my two kids. We were watching it on my computer. And at various times, he just starts smiling. And I think I’ve heard him say in interviews that when he’s really hurting, when there’s pain, he smiles. He intentionally chooses to smile. Now again, he’s not someone with, to my knowledge, a history of chronic pain, but it’s the same idea, isn’t it? He’s kind of almost trying to battle or buffer the pain by changing his experience of it.
DR. HOWARD SCHUBINER: Yeah, if you’re interested in running, the book by Chris McDougall called Born to Run is amazing. I love it. Amazing book, not Bruce Springsteen, Born to Run. The Joy album as well. And he talks about the research showing that the more structure the shoes, the shoe companies, the more structure they give, the more people have pain as opposed to the less structure. And he talks about running with freedom and running with joy in that book and how these ultra marathon runners from Mexico do it really in the same way.
And so it’s amazing how powerful our mental experience is in determining how we function day to day in our lives. Now, is there a pushback on this? It is massive. I mean, prepare yourself for letters and people really misunderstanding the idea of the pain being real, of the symptoms, of the suffering being real. And I’ve been there and you’ve been there.
When my mom was dying, I had this horrible upper back and neck pain and it just lasted and lasted and lasted. And when my dad was dying, I had leg pain shooting down my leg and I still get pains now sometimes, even for no reason. And I’m walking around or, you know, I’m going to play golf, which is, you know, supposed to be relaxing, but it’s actually kind of frustrating and humbling.
But the point is, is that this stuff that we’re talking about is really misunderstood. And it’s so easy to take it as it’s all in your head and you’re making it up and we’re mean and cruel people. And on the other hand, the other extreme is that, oh, yeah, you’re incurable. There’s nothing we can do because the chronic fatigue or the fibromyalgia or the irritable bowel or the back pain is totally… you’re going to have to live with it the rest of your life. And what kind of message is that?
So, so horrible. And so, we’re talking about a new way of dealing with these disorders, which are the major cause of disability worldwide by far. The major cause of disability worldwide is chronic neck and back pain, headaches, anxiety, depression, irritable bowel, fibromyalgia, etc., etc., etc.
The Connection Between Chronic Pain and Mental Health
DR. RANGAN CHATTERJEE: I think I heard you in an interview once say that the increasing prevalence of chronic pain has mirrored or certainly followed the increase in anxiety and depression in society.
DR. HOWARD SCHUBINER: A hundred percent. And there’s a great study on that by Tim Brown from Berkeley. And he took in the US, he took Berkeley, California. He took nationwide data on stress and anxiety in the country following 9-11, 2001. And you could see it rising up over those next couple of years. And then he took data in the country on back pain. And you saw it mirroring, rising up in the same, exactly the same. And then as the stress went down after a couple of years, I think it was, the back pain started to go down a little bit before.
Back pain has doubled in the US in the last 20 years. Backs haven’t changed. Our backs haven’t changed. But the rates, and we know anxiety and depression are soaring as well. And in this pandemic era and the polarization era and the political era, everything is just getting worse because of the simple fact that our brain creates what we experience.
DR. RANGAN CHATTERJEE: Tell me about repetitive strain injury. Because as you said, back pain is going up, neck pain is going up. And much of the time it’s put down to posture. And the fact that we’re looking at computers and phones and… What’s your view on that?
DR. HOWARD SCHUBINER: Yeah. There’s a lot of research that’s been done on posture. And the bottom line is posture matters, but not very much.
You know, if you’re hunching over a computer, yeah, if you sit in that way for a couple of hours, your neck is going to be sore. Of course, it’s going to be sore. Everyone’s neck is going to be sore with that. But it’s not going to cause chronic pain unless something else is going on in your life. The fear of it, the worry about it, the newspaper articles about posture and sitting up straight and everything that’s scaring you, plus the stress that’s going on in your life, all that can feed into this repetitive strain injury with typing.
You know, it’s like, okay, we’re typing. I mean, if you look at the actual effect of typing, you’re moving the fingers a little bit. Remember type, well, you’re too young.
DR. RANGAN CHATTERJEE: I remember typing like this.
DR. HOWARD SCHUBINER: My mom had one. And people, mainly women, were in these positions of typing eight hours a day on these things where you really had to bang on the keys. They didn’t get repetitive strain injury.
There was an epidemic of RSI in Australia in the 80s. It started rising, people talking more about it. This is very well documented and people writing about it and doctors diagnosing it. The rates just kept going up and up and up. And then finally the government said, what’s going on? We’re not paying for that.
DR. RANGAN CHATTERJEE: It makes me feel, is there an unintended consequence of doing this? I don’t just mean with mental health, I mean with everything. You want to raise awareness of things. You want to raise awareness that emotional pain, emotional things that we haven’t processed can cause physical pain. But there is probably a sweet spot, whereas if we start talking about stuff too much, saying, oh, that loads of people have got RSI, your posture and your computer’s causing problems, you hear that more, that becomes your reality. There’s a potential problem there, isn’t there?
Cultural Influences on Pain Perception
DR. HOWARD SCHUBINER: Well, there’s been a long, long history and there’s a great book by Edward Shorter called From Paralysis to Fatigue, where he examines the history of psychogenic type illnesses over the last couple of 200 or 300 years. And he talks about how in different societies, different symptoms tend to arise as a cultural phenomenon. Right now, anxiety and depression are cultural phenomenon.
Young people, look at the rates of anxiety and depression in teenagers now. The rates of back pain, there was a study recently where one third of teenagers reported having back pain. And when I studied pediatrics and internal medicine, when I studied pediatrics, no teenagers had back pain. It was unheard of. If a kid had back pain, it was an emergency situation because there was some major problem.
And so I have a friend who’s from Iraq, he’s a physician. And he’s here, we were talking, a great guy. I was saying, you know, what was surprising about you when you came to the US about medicine here? And he said, back pain. And I said, why is that? He said, well, people didn’t have back pain in Iraq or Jordan, where I practiced. It was very uncommon. People had stress, but their stress was manifest in different ways because culturally, there were different outlets for it.
DR. HOWARD SCHUBINER: And so when we think about these things on a societal level, and we think about how people are treated, how we treat each other, the major thing that in longitudinal studies of people in workplaces, like factories, the people who are more likely to develop musculoskeletal pain who are workers in a factory are those who are being treated poorly by their management. And that’s been shown, not how much work and physical activity they’re doing, how they feel about their work and how they’re being treated.
DR. RANGAN CHATTERJEE: Did you not share a study once, I think, about how well back surgery is going to go for you? Something like that, I think.
DR. HOWARD SCHUBINER: There’s a study on how well back surgery will go for you based on childhood adverse events. So people who had zero, you know, according to the ACE scale, right, the adverse childhood events scales that Fellini put together in the 90s, people at zero had 85% chance of having a successful surgery for their backs.
People with one to two had one to two of these adverse childhood events, like abuse, neglect, alcoholism in the family, etc. One to two had 75% chance of having successful back surgery. If they had three or more, they had 15% chance of having successful. And there was no difference in the surgeries or their backs. This had to do with adverse childhood events being powerful forces that were still affecting them all those years later.
DR. RANGAN CHATTERJEE: What you said about culture and how we have different cultural expressions of our stress and our emotions, it really rings true that. And I think it’s something that medicine, you know, and I’m obviously biased by my experience here in the UK, because that’s where I practice, that’s where I’ve trained. I’m not sure we take that seriously enough because we get taught how to take a history.
We ask a certain set of questions. That’s great if the patient has the same understanding of what those questions are designed to elicit. Great then. But for example, in some cultures, they just don’t have a word for indigestion. It just doesn’t exist. If you don’t have a word for indigestion, you may be suffering from something, but it may manifest in a different way, in a different physical symptom, a bit like your colleague from Iraq was saying about back pain.
DR. HOWARD SCHUBINER: Yeah, there’s been some studies about, I think the word is granularity in language and how people use language in a granular way, meaning more granular, meaning having, oh, well, is it an ache or a sharp or a hurt? Or is it on an emotional level? Is it more rage or contempt or annoyance?
Or, you know, the language that we use for things can be very specific and granular, but it can be very broad. It’s like, it just hurts. You know, it just feels bad. Yeah. You know, it just feels bad. But that’s communicating. There’s something bad. There’s something bad.
And that’s if we have an open mind to looking at, on one side, the medical and the structural, but also on the other side, the psychological and what people have to cope with and deal with in their life. It makes sense. Yeah, you feel bad. Well, let’s, you know, we’ll do some tests, make sure there’s nothing actually structurally wrong. But what does this bad, what does that mean bad? And what’s going on in your life that might make you feel bad? Maybe we can’t change or maybe some things can change.
A lot of things you can’t change in life. But how can we help you be more at peace? And like, I don’t just, when I say those words, I think about, you know, your dad, you know, going into the, it’s, there’s a peacefulness and maybe he was at peace as well. If there’s, if we can somehow find, find peacefulness, you know, in our lives. And if we can somehow find peacefulness in our societies that are so, so torn apart, that’s what’s causing suffering.
But it’s manifest in this physical ways and go to doctors, like doctors are the ones to solve these problems. Doctors are not well equipped. I was in Australia last week and giving a lecture and there was a GI physician there. It spent his whole career seeing people with irritable bowel syndromes and doing diets and medications and things like that. And he heard my lecture and he said to me, Howard, you know, your lecture was depressing to me. And I go, why is that? He says, well, I realized that I’m very ill-equipped to care for these patients. I don’t know how to do that because I’ve been trained in this whole other way.
DR. RANGAN CHATTERJEE: But that, what he said though, I have a lot of respect for because at least he had the courage to say that and accept that and acknowledge that. You know, it’s interesting, Howard, this morning, and this was in preparation for talking to you, I phoned up one of my best mates, Steve, who is a brilliant spinal surgeon on the south coast of England. And I said, hey, mate, listen, I’m talking to Howard Schubiner later. We’re going to talk about chronic pain. You see a lot of pain. In your view, what is the most important therapy you give your patients with chronic pain?
Because, you know, he’s a super specialist, you know, people who’ve got chronic pain who can’t get by to get referred up to him. And he said to me, he said, the most important thing that I do for my patients when they come in to see me is I listen to them and I show them empathy. And it was really profound for me to hear that.
The Brain’s Role in Chronic Pain
DR. HOWARD SCHUBINER: I mean, he’s a great guy. He’s a brilliant surgeon. He goes, look, surgery is great for acute cases where we can see something’s going on. But for a lot of the time, we just don’t need to do it for these people with pain. What they need is to feel heard and validated because often by the time they come to me, no one has ever heard or validated their pain, their symptoms, that it was real. And he goes, the truth is with chronic pain, for me as a surgeon, it’s a lot more touchy feeling.
That’s exactly what he said to me. And he goes, all kinds of things kind of work. But what I can offer is honesty, but the surgery probably will not help them. And then listen and empathy. And I thought that was really powerful.
DR. HOWARD SCHUBINER: Yeah, I mean, don’t do something just to do something because you can make it worse. There’s a saying in surgery, when you operate on pain, you get pain. But to be honest and to be open and to be empathic and now what we’re saying is that this touchy feely stuff, it’s not hocus pocus. It’s not what we would say, woo woo. It’s neuroscience. And we’re talking about the neuroscience of the brain and why these things happen.
And we have data showing that people can get better and we have data and we have techniques and we can train doctors and we can train therapists. If you’re a psychotherapist, a psychologist or a social worker doing therapy, 50% of the people coming to you for anxiety or depression also have a chronic pain condition. And the question is, who should be caring for these people with chronic pain?
It should actually be the therapist, the behavioral health people, because they can take the time and they can develop the skills. Your surgeon friend doesn’t have the time. He has the skills to be honest and have integrity and not operate on what he shouldn’t and to be caring and empathic and listen.
He can do all that. But he can also learn how to talk this language of the brain causing pain, how to assess and say, oh, your pain is shifting and moving. That means it’s not due to this disc here. This disc would cause pain going down your leg. You don’t have pain going down your leg, right? He can tell people that, which that’s what we do, right? In the assessment.
And then maybe he can point them to, there’s a bunch of apps, there’s a bunch of online programs and we’re training physicians and we’re training nurses and psychotherapists and massage therapists and acupuncturists. And we’re training folks how to do this pain reprocessing work and how to do emotional processing work as well.
DR. RANGAN CHATTERJEE: I mean, it’s incredible what you’re doing. And as I’ve already said, you’re doing research, which is giving this a real scientific robustness, which ultimately is what’s needed if we’re going to change the profession. I want to get into some of these therapies and in terms of what people can actually do.
Before we do that, there’s two cases I’ve heard you talk about before, which I think are beautiful illustrations of how powerful the brain is in generating pain. One was, I think, a chap who had been in the Vietnamese war and 20 years later, something happened on a street. The other was a UK construction worker. I don’t know if you remember those cases. Would you mind sharing them? Because I think they beautifully illustrate this.
Three Powerful Pain Stories
DR. HOWARD SCHUBINER: Yeah, of course. I always tell the three pain stories. The first pain story is a friend of mine who was at a construction site alone, shot a nail gun, shot a nail in his hand, had no pain.
Why did he not have pain? He has a nail in his hand. Well, I don’t know why his brain decided not to turn on pain at that moment. Probably because he was all alone. His brain had to decide, look, be in pain and suffer, or drive to the hospital. His brain said, drive to the hospital. I mean, you know, I can’t speculate why that is. But he had no pain.
DR. RANGAN CHATTERJEE: He had no pain at all. Yeah, exactly.
DR. HOWARD SCHUBINER: So, not all injuries cause pain. Okay. Number two, it’s a guy in Britain, a construction worker, jumps off a scaffolding onto a nail sticking up in the ground. The nail goes completely through his boot. He can see the nail sticking out on the other side of his boot. He starts screaming in pain. He has severe pain. They rush him to the hospital. They give him IV pain medication when he gets there. And they take his boot off and the nail is right between his toes. There’s no injury at all.
Is his pain real? Yes, because all pain is real. All pain is created by his brain. And his brain predicted, and the science of the brain is called predictive processing. His brain predicted that he should have pain based on the nail. It just made an error. But it created this pain and the pain is real.
Never underestimate the power of the brain to create severe symptoms, severe pain, severe fatigue, severe seizure type activity that we see all the time that’s due to the brain called paroxysmal non-epileptic attacks. We know that because people are having these looks like seizures. And the neurologists, they know how to treat seizure disorders, but they put them in the EEG machine while they’re having the thing. They monitor them. And then the EEG is totally normal while they’re having this seizure activity. It’s not a seizure. They don’t need medication. They need to understand that they’re not actually damaged. They need to do these kinds of therapies we’ll talk about. That’s the second case.
And the third case is the guy, again, somebody I met, who happens to be a physician now, but he was in the Vietnam War as a young man and he got injured with shrapnel wound. A lot of guys died. It was a lot of gore. And he got helicoptered out, medevaced out. So he had pain from the shrapnel wound.
What happened to his injury? They healed. Why? Because all injuries heal. So his injury healed. Now, did his brain turn off that danger signal and make his pain go away? Yes, he was fine. He was pain-free. But for what, 15, 20 years?
Yeah, 20 years later, he’s walking down the street. He gets startled by the sound of a helicopter in the sky. And all of a sudden, he gets the same pain in his leg that he had had 20 years earlier. That neural circuit for pain had been learned, had been remembered, and then had been activated through a triggering response.
And that’s part of our assessment that we do to help people see that, gee, why is your pain occurring when you sit in that chair, but not that chair? Why is your pain occurring when the wind blows? Why is your pain occurring when the weather changes? Why is your pain occurring in cold? Or why does it go away when you take a shower? Why does it? All these changes that we’re looking for to demonstrate these neural circuits. So this understanding of how the brain works and predictive processing is critical. And we’re not taught that in medical school.
DR. RANGAN CHATTERJEE: We have very, very powerful cases to just illustrate what you’re talking about, about the brain generating the pain. It’s all the brain. So we need to retrain the brain to eliminate it and help people heal.
Now, I know so many people will be suffering or they’ll have loved ones who are suffering with some of the chronic pain symptoms and conditions you’ve mentioned. I would strongly recommend your book, Unlearn Your Pain. That’s for patients, isn’t it? That’s for people who are struggling. I think it’s really easy to read. It’s got the research. It’s got some really great practical exercises. And I think you also train healthcare professionals. Where can people find out about that?
Resources for Pain Management
DR. HOWARD SCHUBINER: Yeah, absolutely. We do have a book called Hidden From View, which is for professionals. We also have two other books we’ve written that are compendium. One is a textbook of psychophysiologic disorders. That’s available through the Psychophysiologic Disorders Association. Here in Britain is SIRPA, S-I-R-P-A.org.
That’s brilliant, yeah. Yeah, they do great work here. And then we’ve got trainings that we’re doing virtual, live and recorded trainings. We just launched a mobile app to train people. It’s called OvidDX.com.
DR. RANGAN CHATTERJEE: Okay, OvidDX.com.
DR. HOWARD SCHUBINER: That’s the name. Ovid, you know, was a Roman poet who wrote, when the mind is ill at ease, the body suffers. That was one of his quotes.
DR. RANGAN CHATTERJEE: And it says it all. A big theme throughout this conversation is that emotions, unprocessed emotions that get stored inside of us that we don’t do anything with, can, in some individuals, generate pain.
Breaking the Pain Cycle
DR. HOWARD SCHUBINER: Correct. What happens is we respond normally with fear of them. There are six Fs. Fear of them, worry about them, worried of what’s going on, focus on them, paying attention, monitoring all the time, fighting them, trying to push back, which gives them so much power, frustrated by them because we’re angry and upset, trying to figure them out, going to all sorts of practitioners and therapies, and then finally trying to fix it. But the harder we do all those things, that gives the brain the message there’s a problem and it makes it worse.
So this vicious feedback cycle of pain and other symptoms leading to these responses, the six Fs, fear being one of the most important, leading to more pain. So when we interrupt that cycle, which you did when you lifted your mom that time, when you told yourself you were okay and you smiled, you interrupted that cycle. You just interrupted that pain cycle by giving the danger signal in the brain these calming and safe messages. And that’s what pain reprocessing is at its core.
And we’ve got a whole bunch of techniques of how to do that so that people can do this, do this, do this, change your relationship to the symptom and see what happens. And then when you start seeing, you start investigating, looking, oh, hey, it hurt then, but it didn’t hurt then. Oh my God, it is my brain. Oh my goodness, I’m going to be okay. And then there’s that relief.
DR. RANGAN CHATTERJEE: I imagine even that knowledge alone, even if you do nothing else, even when the penny drops inside you that, wait a minute, this is nothing serious physically, this is not anything structural, I’m okay. Like even that must also help in and of itself, I would imagine.
DR. HOWARD SCHUBINER: Well, I started this work in 2002 and I read a book by John Sarno, Dr. Sarno, right? And Dr. Sarno has passed away. I just got an email from his daughter yesterday and she’s a therapist and she’s doing this work, carrying on.
And anyway, it was a beautiful email and he taught me and I’ve been doing this for almost 20 years now. Well, I guess 20 years. And his books are still bestsellers. Dr. Sarno’s books would state this and he was brilliant in how he thought about it. He keeps getting bashed. Everyone loves to bash Dr. Sarno. So I’m here to… He wasn’t right about every little detail, but Einstein wasn’t right about every little detail. Come on.
Anyway, but people will read his book and then the pain will go away, just from the knowledge. And it’s called The Book Cure. And it’s happened many… And there’s a documentary on Dr. Sarno. There’s a couple of documentaries to mention. One is on Dr. Sarno called All the Rage, produced by Michael Galinsky. It’s great. It’s just a great picture of him. And then there’s a documentary Kent Bassett and Marian Cunningham made of my work called This Might Hurt.
So there’s a couple documentaries out there and there’s a new one coming out soon, hopefully called Brain Pain, which was a documentary done about the boulder back pain study that I was telling you about. So there’s some films that people can watch to really kind of get a first-hand glimpse of some of this work. But yes, the answer is yes. Just knowing that you’re okay can maybe 10, 15% of people just turn off that danger signal.
Mindfulness and Pain Management
DR. RANGAN CHATTERJEE: What are things like journaling and meditation fits in here?
DR. HOWARD SCHUBINER: Yeah, so once you’ve done the understanding part of it, and then you start doing this pain reprocessing part of it, lowering the fear reaction, beginning to start moving again and challenging any of these triggers by smiling at them. It sounds silly, but the pain is not the enemy, is their message. So if you have a child lying in bed fearful of a monster in the closet, you’re not going to be mad at the kid, hopefully.
You’re going to open the closet door, say, look, there’s no monster. You’re okay. Lie down with them. Tell them you love them, that you’re okay. Read a story, get them to laugh. They’ll go to bed, right? That’s how we’re treating the brain because the brain is just fearful. It’s worried about you in the sense of causing these symptoms. When a kid falls off a bike, they look to you to see if they should cry or not. And if you freak out, they cry. But if you smile and say, oops, that was fun, then maybe they don’t. So this is this pain reprocessing part.
Now, meditation can fit into that because we use mindfulness meditation type practices in this work. And mindfulness, I’ve been teaching mindfulness since 1999 and everyone should learn mindfulness. There’s no one who’s studied mindfulness who doesn’t agree with that. Children, everyone should learn it.
But the fascinating thing, Rangan, is that in research studies, mindfulness has not been particularly helpful in reducing chronic pain. Why is that? Cognitive behavioral therapy is not particularly helpful. Acceptance and commitment therapy, not particularly helpful in actually reducing chronic pain in randomized controlled trials. Why is that?
Because none of them are doing the first step of the assessment of categorizing the pain into a neural circuit problem as opposed to a structural problem. So when you do mindfulness, you’re noticing your sensations in your body, but it hurts. It’s painful.
Reframing Pain as a Brain-Created Experience
DR. HOWARD SCHUBINER: It’s uncomfortable. And you’re interpreting those sensations as being dangerous because there must be something wrong with you. You’re not getting better.
You have to reframe first. Yes. You have to recategorize the symptom into basically, and this again, I’m doing this with saying this word with love and compassion.
And the reality is that the symptom, this pain or whatever it is, is basically a thought. It’s basically created by the brain. And now if you can observe that, now you can step back from it and observe it and just watch it and not try to fight it and be frustrated by it, but set that aside and then be with it and see what happens.
And then maybe it shifts. Maybe it gets a little worse. Oh, my brain just made it go up.
Oh, that’s interesting. What’s going to happen next? Oh, it just went down.
Oh, that’s interesting. Oh, it moved over here. And all of a sudden you see, and then it really, as you said, it drops.
All of a sudden you get it. And then so meditation has a really important role in this, but not just meditate. Understand and use the tool in a way which is going to help reverse the pain as opposed to cope with it.
DR. RANGAN CHATTERJEE: There’s studies on yoga, I think as well, aren’t there? That yoga, deep breathing practices, whether it was part of yoga or not, can help change our perception of pain. I think there’s quite a lot of studies on that.
DR. HOWARD SCHUBINER: Sure, of course, because what you’re doing is you’re making yourself feel safer. You’re calming the danger signal, you know, the autonomic nervous system responses and all that sort of stuff. You’re calming it and you’re giving yourself a sense of control that you can do something.
Yoga, of course, is beautiful because you’re pairing that with movement. You’re pairing the calming and the reassurance and the joy with moving your body. So neurons that fire together, wire together.
So when you’re moving with fear, you’re reinforcing these neural circuits of pain, fear, pain. But when you start moving gently with calm or with joy or with control or with peacefulness, now you’re training your brain that these movements are not dangerous and those neural circuits start to get ingrained.
The Connection Between Emotions and Chronic Pain
DR. RANGAN CHATTERJEE: I’ve wrote down this quote that you have written in an article. “Over the past decade, I’ve learned that migraine, along with other related conditions, such as chronic tension headaches, pelvic and abdominal pain syndromes, chronic neck and back pain are often caused by a combination of life events and emotions that are neither expressed nor processed.” All of these conditions are associated with early onsets of, I think, symptoms which sensitizes the danger signal.
DR. HOWARD SCHUBINER: Early onset of stress, like adverse childhood events, probably.
DR. RANGAN CHATTERJEE: Which sensitizes the brain. That’s the key, isn’t it? It sensitizes the brain.
And as you say, the yoga or the deep, slow breathing is switching off the stress signal saying, hey, I’m safe, I’m okay.
DR. HOWARD SCHUBINER: But then we can get into the emotional side of it because you mentioned journaling. So journaling is part of the techniques that we would use on the second part of the treatment, not the pain reprocessing part, but the emotional awareness and expression therapy, which we’ve developed and worked on. It has components of intensive, short-term dynamic psychotherapy that my friend and colleague, Alan Abbas, is the foremost researcher and teacher in the world on that.
Plus some internal family systems work as well. So if you put kind of those things together, you start to deal with the emotions of it. And that’s a whole other area that can really lead to healing, healing on the inside.
Not just recovery from the symptoms, but using the symptoms as a way to decide what’s important in your life. So that’s a whole other area that we can discuss as well.
Personality Types and Chronic Pain
DR. RANGAN CHATTERJEE: How much does our personality type influence whether we’re going to suffer with chronic pain? And I guess why I’m thinking of that is if early life trauma, if ACEs are hugely influential in what’s going to happen later on in life, including with chronic pain. I’ve had three conversations with Dr. Gabor Maté on this show about how our childhoods can affect our adult experiences, how we are when we get triggered by our partners, all kinds of different things. But often we develop certain traits, certain personality traits that are not really who we are, they’re who we became to get through childhood. So poor self-esteem, so being a people pleaser, wanting to do things for other people, right? Those personality traits, as I believe, as Gabor believes, are not necessarily who people are or who they have to remain if they go and do the emotional work.
So I have to go, oh, actually, that was a defensive mechanism that I took on to help me through childhood. I want to let go of it now that I’m in adulthood, it’s no longer serving me. Do we see patterns?
Have you seen patterns in your clinical practice of certain types of people who tend to be the ones who suffer with a lot of these chronic pain syndromes?
DR. HOWARD SCHUBINER: Yeah, there’s no question about that. There’s really kind of three ways to think about it. One way is we are actually born not blank slates.
There’s been really nice studies of children and temperament, so to speak. Some kids are more sensitive than others. Some kids are shyer than others.
You can breed sensitivity and shyness and fearfulness into mice by doing genetic breeding studies. So there’s some stuff that we actually are born with. But the longitudinal data on that shows that those change over time.
Some kids are very sensitive. My daughter was super, super sensitive as kids. Now she’s lecturing around the world.
So there’s that. But what you’re addressing is more important, which is the acquired personality traits. And those are highly connected to later life pain and other of these type of neural circuit type problems, for sure.
And the reason is, is like you say, they’re adaptive. You know, if your dad comes home every day and sometimes he’s really nice and kind and sometimes he’s really angry and critical, you learn to be on edge. You know, you learn to be a people pleaser.
If your sibling is sick and they’re getting all the attention in the family because they’re sick, they’ve got leukemia or they’ve got bad asthma or whatever, they’ve got a mental illness. Well, you learn to get into the background and be a people pleaser and be a perfectionist and be always being good and putting yourself last because everybody else matters first. And these are adaptive techniques that get you by.
But when you get on into adulthood, sometimes your brain is going to say like, what about me? You know, what about you? How come you’re putting yourself last all the time?
And that’s putting more pressure on ourselves, more pressure on this danger signal. And so that is an important component of this situation or this condition that oftentimes people, as you say, can address and you can begin to change in them. So it’s not that you shouldn’t be good or you shouldn’t be kind.
It’s just that you also have to stand up for yourself sometimes. Sometimes you have to learn to say no. It took me until I was 50 until I could say no.
It took a long time.
DR. RANGAN CHATTERJEE: I think it maybe took me until I was about 42. So hopefully the generation below us will start to do it earlier.
DR. HOWARD SCHUBINER: I like to say it’s a magic word. It has two letters, an N and an O. But not every…
I mean, it’s the human condition to have some of these things, of course. So it’s just part of the mix. And each person is unique and individual in terms of how that mix plays out in their life.
The Role of Pain Medications
DR. RANGAN CHATTERJEE: I always think what you’re doing with your clinical work, with your research is a great service to humanity. There are so many people struggling with this. This is a topic we’ve never really covered on the show at all.
So I’m so delighted that we finally got to cover chronic pain in all its many different forms, in all its different guises. I feel that what you have done certainly to me is help people feel less alone. But actually, no, no, your pain is real.
Yes, maybe your doctors haven’t found anything structural. Maybe you think you’re going crazy with pain. But you’re not.
It’s just that no one’s helped you yet get to the root cause. If you want to solve anything, you need to get to the right cause. I’m hoping there have been some penny dropping moments for people in this conversation.
There are a lot of people, Howard, who, well, what do painkillers fit in here, in your view?
DR. HOWARD SCHUBINER: Well, when people are suffering, we want to alleviate suffering. I mean, that’s part of being a physician, part of being a caregiver. So Dr. Sarno kind of had an idea. He wanted people to throw away their pills, throw away their crutches, throw away the things that are helping them cope, which is fine when you have that amount of confidence. And it’s not too bad. But some people need pain medications, certainly if they have ongoing, if you have a metastatic cancer kind of situation.
Doctors have gotten worried about giving pain, strong pain medications to people who are dying of cancer. I mean, that’s silly. Why should we not alleviate suffering in that way?
And if someone’s suffering with severe pain due to a neural circuit type problem, they may need pain medications while they do this work, certainly. And so I don’t want people to feel like they can never take a pain medication. But if you can alleviate pain with pain medications temporarily while you start investigating your life, while you start the pain reprocessing work, while you start dealing with some of the emotional situations in your life, then over time you can reduce the pain medication.
One of the problems we’ve had in the medical profession recently is people are put on forced reductions of opiates and saying, okay, you’re going to taper. And what happens is now you get what’s called, as I’m sure you’re aware, the nocebo effect kicking in. So people are fearful that their medications are being taken away from them forcefully.
And now the pain is going to be worse because the brain is put into a bigger state of fear and lowering the medication is much harder. So what we try to do is we try to first, just stay on your medication. Let’s see if we can get you out of pain first.
If we can get you out of pain using these methods, then tapering that medication is going to be easy.
DR. RANGAN CHATTERJEE: I guess this speaks to personalization, doesn’t it? If a patient rocks up at your door and they’ve been on painkillers for 10 years, they think that they’re helping, you got to take a different approach from, let’s say, someone who’s coming into you for the first time where with this new information, hopefully you can actually set them on a different path. And I think this is why I think healthcare professionals need to understand this stuff because we can be hugely influential in what that patient believes when they walk out that door.
I’ve always said like, you know, migraines are really common. You know, my preference is always to try and help patients get to the root cause so they don’t need any medications. But sometimes a patient, you got to meet them where they’re at, first of all.
And sometimes it is so bad that maybe in the short term, you give them something, but you also need to make it clear in my view that, hey, listen, this medication is not going to help us get rid of this. It’s simply going to help you manage this so you can tolerate your work at the moment. But I can also help you if you want, try and find out what’s causing this.
I don’t think that second part of the conversation is often had. I know the time of consultations, certainly in the UK, doesn’t make it any easier, but it’s not just that. It really, it’s not just time.
I think time’s the easy thing to say. It does play a huge role, but I think our understanding is simply not there as well for this. I don’t know about you, Howard.
I’ve often found with some of these patients in chronic pain though that they’re taking huge amounts of medication and they’re still in pain.
DR. HOWARD SCHUBINER: Right, right, for sure. What we’re doing is the band-aid technique, the coping technique, and we keep adding on to that more and more and more. And we need a different path.
There’s no question about that. But we can’t force this path on people either because you said the words, if you want. If you want.
If you want. Because what we’re doing is we’re offering, and we’re, as you say, we’re meeting people where they’re at and we’re meeting with empathy and kindness and caring and understanding. And a lot of people, not a lot, I mean, most of the people who come to me understand this.
That’s why they’re coming to me as a physician. But, you know, sometimes they don’t or, you know, it doesn’t really make sense to them. And I’m like, fine, you know, this may not be the right path for you.
There are lots of other paths to healing. There’s lots of other ways of healing that could be, you know, all sorts of stuff in the alternative fields or whatever. I try to be careful of that.
And I try to help people not spending too much money or, you know, getting on other diagnoses that don’t make sense. But there’s lots of other paths to healing. And maybe there’s other medical paths that you haven’t tried yet.
Let’s sort it out, you know. Isn’t that what you say here? Let’s sort it, you know.
And let’s just take it step by step. And let’s see what happens. And let’s investigate.
Once you have this kinds of information, now you can look at what’s happening over time. And you can look for those experiences that you can have which show that, oh, the pain, this happened in my life and the pain went up. Or this happened in my life and the pain went down.
Understanding Pain Through a Different Lens
DR. HOWARD SCHUBINER: Or it’s inconsistent. Why is it happening sometimes and not other times? And now that you have a framework for understanding that, you can say, hmm, maybe it is my brain after all. Wow, wouldn’t that be something?
DR. RANGAN CHATTERJEE: Hello, this podcast is called Feel Better Live More. When we feel better in ourselves, we get more out of our lives. And clearly, pain is something that makes people feel worse. It affects every single aspect of their lives. For people who are listening, who are watching, who are struggling in their lives, they’re struggling with pain, or someone close to them is suffering with chronic pain, do you have any final words for them?
DR. HOWARD SCHUBINER: Well, I think the starting point has to be compassion and caring and understanding. And if we can strip away some of the fear and some of the pejorative words, and “it’s all in your head,” if we can strip away the way that sometimes people are treated, and being treated in that pejorative way, but if we can also strip away some of the diagnoses and some of the words that people have been given, like “incurable” and “bulging discs,” and all the names, oh, it’s chronic fatigue, and there’s so many names, I don’t know if we have time to get into it, but so many names have been given to people. “Oh, you’ve got chronic Lyme disease, you’ve got Ehlers-Danlos syndrome, your posture’s all bad,” all these things, if we can just start over, strip away the unkindness and strip away the “incurable,” and start in a middle place with investigating carefully and taking time to look at people’s lives and look at their symptoms and see what you can find. Because when you do that, usually you’ll see, maybe there’s something here that we can work in.
DR. RANGAN CHATTERJEE: Yeah, just on that point, you mentioned chronic fatigue, chronic Lyme disease, these kind of things, and I don’t want anyone to go away from this conversation feeling at the end that, “Oh, so I don’t have that,” or, “I do have that, and Howard has just said, forget about that.” I think it’s really important that we help people understand that. What exactly did you mean by that? Did you say those things are not helpful, or are you saying that, look, if you’ve had that for a while, temporarily, why don’t you just park that, start again from scratch, evaluate it as if nothing had happened before? What exactly did you mean?
Rethinking Chronic Conditions
DR. HOWARD SCHUBINER: Yeah, let’s evaluate it. Like I say, as physicians, everyone needs an individual assessment. And do you really have, is it really chronic Lyme? Let’s look at the tests and let’s look at the symptoms.
You know, with long COVID, there’s a lot of research on that now, research showing that people with preexisting anxiety, depression, loneliness, fear, are more likely to get long COVID than those who don’t have that prior to getting COVID. There’s research showing that people who didn’t have COVID had as high or higher rates of long COVID as people who actually did have COVID in a big, large French study.
And if you just take each person as a unique individual and just look at them, talk to them, do the testing, you know, if there’s no explanation for it medically, and the symptoms are brain fog and fatigue and aches and pains and diarrhea and headaches and anxiety and depression, it’s all there. What’s the harm in looking at it closely and looking at it from this lens of neurocircuitry? What’s the harm in just looking at it?
You know, I had a patient who had long COVID. Young woman had it for about a year and a half, really bad. And she saw me, just one visit. And two weeks later, she was 80% better. It was amazing. But what was really interesting is she had loss of taste and smell, which is part of COVID, right? You get COVID, you get loss of taste and smell. That’s got to be a structural problem, right? I mean, how could it not be?
Well, she had loss of taste and smell for 18 months. And then I saw her one day. And then the next day, her taste and smell returned. And then the day after that, it was gone again. And then it returned again. And then it was gone again. Her brain had the capacity to turn on and turn off this thing which seems completely neurological. And it’s certainly real. But the power of the brain is immense.
And if we’re just open to that, that’s all I’m saying. I’m not judging people or assuming that what they have because of their label is or isn’t real. But it’s taking the time to investigate it in a careful and compassionate way. That’s what I’m trying to say.
DR. RANGAN CHATTERJEE: What did you do with that lady?
DR. HOWARD SCHUBINER: Oh, well, just what we do every day. We went over her whole life and the story linked stressful life events to her situation, looked at the symptoms that she was having, the brain fog, the fatigue, all the testing that she had, making sure that there was nothing structural wrong. And then we started having her change her relationship to her symptoms, knowing that she could get better. Yeah, starting to smile, starting to move, starting to reassure herself little by little.
And then she saw the symptoms shift, get better, get worse. And she said, “Oh my God, it is my brain.” And then they started getting better.
A Fresh Approach to Healing
DR. RANGAN CHATTERJEE: Yeah, so powerful. Whenever I am faced with a patient who’s accumulated lots of different diagnoses and labels, I will often take that approach. Okay, let’s just put them to the side for a minute. Let’s just go back to basics.
I did this very publicly on BBC One in 2016 with a lady who I’ve actually spoken to on this podcast in the past who had fibromyalgia, she had ME. She had, I think, 10 different diagnoses, including anxiety, IBS, depression. She had everything, all the buckets that we can give you in modern medicine. She had been given all of them. She was on 20 pills a day.
I’ve got many other cases like this, but this is one that the public saw, millions of people saw this case. And I remember saying to her, with the cameras rolling, “Look, let’s just put them to the side. You know, you’ve picked up all these kind of carriages and you’re walking around your life with them. You’re on 20 pills a day. You’re still in pain. You can’t work. You can’t be a mother. You can’t be a wife the way you want to. Let’s just start from scratch. Let’s just focus on you as an individual. Let’s start creating health in you.”
And so, this is often how I approach things. Instead of, it’s not saying that those are all wrong. It’s just saying instead of focusing on what’s wrong with you, let’s just see how I can help create health in you with emotional stuff, sleep, stress, movement, whatever it might be. And six weeks later, she was pain-free, pain-free. And then two years later, so this is after the show had finished, two years later, she’s on zero pills a day.
Yeah, amazing. And I said that you will have seen this many times in your clinic, but I say this to leave people with a message of hope at the end. It’s not that we’re saying that’s not real. It’s just saying maybe we need a kind of different approach.
DR. HOWARD SCHUBINER: Yeah, yeah. The power of the brain is immense. The power of our connection to each other, our social connection, the power of what goes on in our lives is immense and has tremendous impact on how we live day to day.
And there’s just so much suffering in the world, so much suffering that I think we can do better. And I think we’re just trying to point the way, little by little, step by step, to doing a little bit better. And you’re doing this work and you’re helping in your work and in this kind of work.
And everybody who sees this work, every patient that I see, they ask this question, “How come my doctor didn’t tell me about this? How come people didn’t know about this? How come I never heard about this in the last five years or 10 years or 20 years of suffering? How come nobody told me that there was a different path?”
And it’s not for everybody. And I don’t expect that everybody who’s listening is going to like, “Oh, yay, we found the way.” But some people will, some people will.
DR. RANGAN CHATTERJEE: I guarantee that. Well, Howard, you’re a huge part of this change in thinking about pain that’s going on all across the world. I hope, like you, that it speeds up and gets out to more and more people, more and more healthcare professionals. Thank you so much for all the work you’re doing. And thanks for coming on the show.
DR. HOWARD SCHUBINER: Thank you. It was a pleasure and an honor. Appreciate it.
DR. RANGAN CHATTERJEE: If that conversation about chronic pain resonated with you, I think you are really going to enjoy this powerful conversation all about the common reasons that many of us feel lost and unhappy.
“Addiction is the most human thing there is. All addictions are attempts to gain pain relief, emotional pain relief or something or another. Then this whole society is so expert at selling us stuff to fill those holes temporarily. This is the whole ethic of this culture.”
Related Posts
- Diary Of A CEO Podcast: on Global ‘Brain Rot’ Crisis (Transcript)
- Diary Of A CEO: w/ Sleep Expert Dr. Michael Breus (Transcript)
- Mel Robbins Podcast: w/ Dr. Amy Shah on 30-30-3 (Transcript)
- Joe Rogan Podcast: #2450 w/ Tommy Wood (Transcript)
- Diary Of A CEO: w/ Louisa Nicola on Alzheimer’s Disease (Transcript)